Credentialing in healthcare is a constant challenge, with regulations shifting and manual processes often leading to costly mistakes. If you’re tired of chasing paperwork or worrying about compliance gaps, you’re not alone.
I’ve seen how the right credentialing software can transform onboarding, automate renewals, and keep audit trails watertight. This article breaks down the seven leading platforms for 2025, covering everything from automation and integration to mobile access and digital credentialing.
You’ll get a clear look at each solution’s strengths, pricing, and best-fit scenarios—whether you’re running a hospital, a clinic, or an online training program. By the end, you’ll know exactly which features matter most for your needs and how to avoid common pitfalls.
If you want to streamline credential management, reduce compliance risk, and make onboarding easier for everyone, you’ll find practical answers here.
What defines the best credentialing software for healthcare?
Understanding Credentialing in the Healthcare Context
Credentialing in healthcare isn’t just ticking boxes—it’s a rigorous process focused on verifying that anyone providing care, from doctors and nurses to allied health practitioners, genuinely holds the qualifications, licences, and experience required to deliver safe treatment. Think of it as the backbone that keeps both patient safety and the reputation of healthcare organisations intact.
So, why is this such a big deal? Credentialing creates the legal and operational foundation for every healthcare provider. Without it, organisations expose themselves to a world of risk: regulatory non-compliance, liability nightmares, and even lost funding from insurers or government agencies. For online learning providers, especially MOOCs in healthcare, credentialing speaks directly to the authenticity of the qualifications they’re granting—a crucial reassurance in an evolving workforce.
Failure to properly manage the credentialing process can lead to significant and costly issues for healthcare organizations, impacting financial stability, compliance standing, and patient safety.
Now, healthcare credentialing lives within a tangled web of regulations. In the United States, for example, compliance frameworks come from the likes of The Joint Commission (TJC), CMS (the Centers for Medicare and Medicaid Services), and specialist professional boards. In places like the UK, bodies such as the General Medical Council (GMC) and Care Quality Commission (CQC) set the standards. These institutions determine exactly what’s required—minimum qualifications, types of licences, how often things need re-verifying, and the audit trails that must be kept.
Within these regulatory frameworks, there's a surprisingly broad set of data points that healthcare organisations need to manage and verify:
- Licences
Government- or board-issued authorisation to practise, absolutely non-negotiable for legal employment. - Certifications
Special expertise or board credentials that show mastery in specific clinical skills or disciplines. - Degrees
Formal proof of education from accredited programmes or universities. - Background checks
In-depth vetting, including prior work history, peer references, malpractice flags, and any issues with regulatory compliance.
Take, for example, the onboarding process for a new hospital doctor. The credentialing team won’t just glance at their medical degree—they’ll need to see specialty certifications, an active licence verified through direct contact with its original issuer, peer endorsements, recent CVs, and perhaps even disciplinary records. And the scrutiny doesn’t end there. After a committee review confirms everything checks out, privileges are granted, and only then can processes like insurer enrolment or patient billing move forward. What’s more, credentialing is never a one-and-done event; monitoring continues well after someone’s hired, tracking expiration dates and ensuring regular re-credentialing as standards shift.
This brings us to a sticking point. Traditional, hands-on credentialing can get ugly fast. Between paper files, spreadsheets, and the constant chase for documents across scattered systems, organisations end up hampered by inefficiency. Inconsistent information, missed renewal dates, and delayed verifications are recipe for stress—and real consequences when audits or compliance checks come around. For both large health systems and online platforms issuing thousands of credentials, these old-school methods are a recipe for admin overload and bottlenecks.
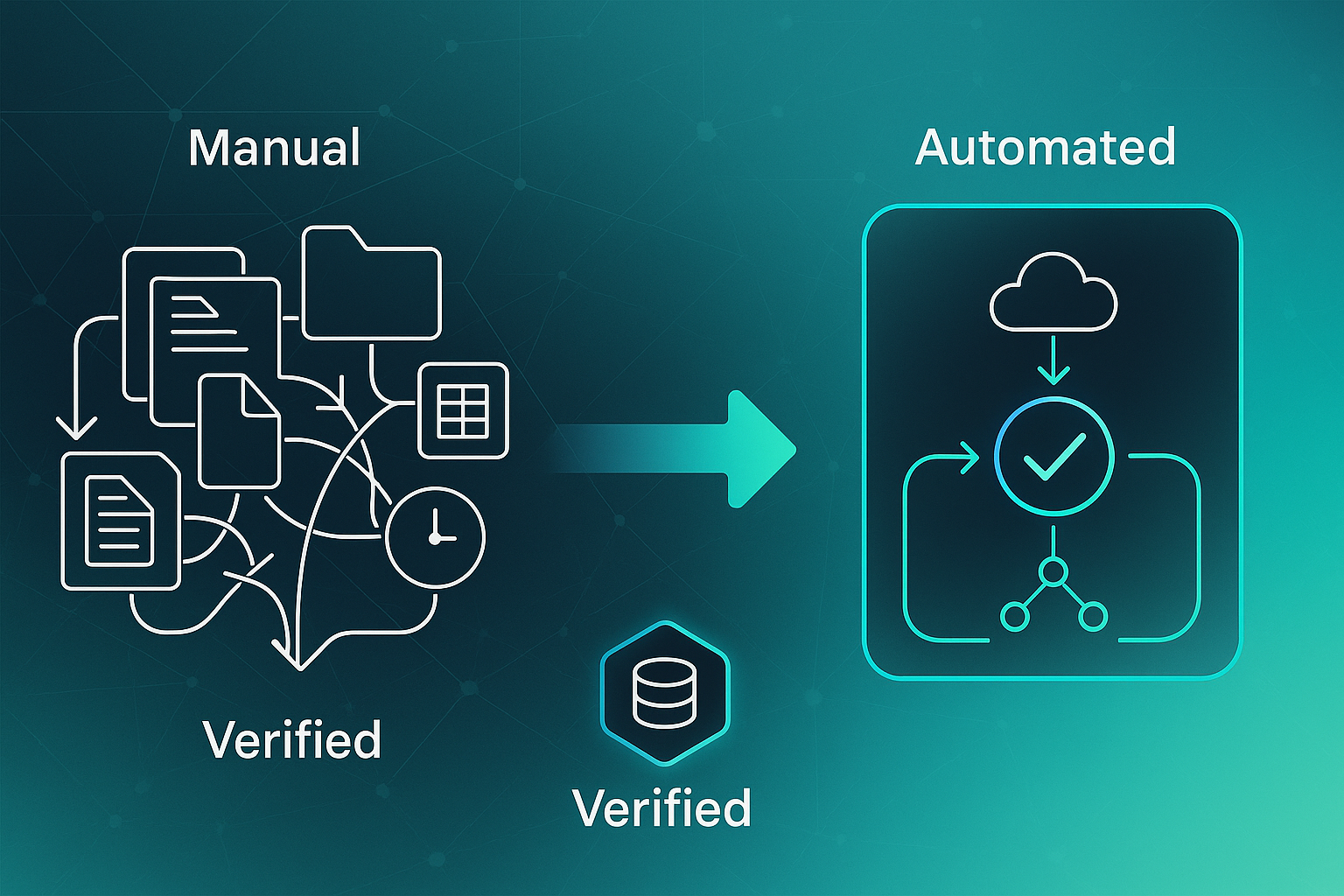
All this underpins why there’s a fundamental shift toward advanced digital credentialing platforms. These systems are not just a modern “nice-to-have”—they reflect both regulatory necessity and the reality that fragmented approaches simply can’t cope with today’s demands.
And just before considering which software solutions really stand out, it’s worth untangling what makes healthcare credentialing platforms different from everything else on the market. That distinction is the foundation for any further evaluation.
What to look for in credentialing software for healthcare
Let’s get into what really sets the top healthcare credentialing software apart in 2025. If you’re aiming to cut down on compliance headaches and speed up onboarding—whether you’re handling a hospital’s staff, or running a massive online training programme—certain features just make life easier. The best systems combine automation, integration, security, and engagement for both admins and providers.
Automated credentialing software can reduce turnaround times by up to 80%, significantly accelerating the onboarding process and time-to-revenue for healthcare facilities.
Core evaluation criteria for healthcare credentialing tools
Here’s the practical truth: finding the right system is about matching its strengths to your biggest challenges. So, what should you be scanning for?
- Automated compliance monitoring
The standout tools auto-generate renewal reminders, and you can tweak those to pop up 90, 60, or even 30 days before a credential expires. They routinely check exclusion lists like OIG and SAM, so you’re covered from a compliance perspective. Audit logs are kept for as long as regulations say you need them. MedTrainer and CredentialStream by HealthStream offer templates that make NCQA audits much less stressful, plus exportable compliance records you can pull when required. - Primary source verification (PSV)
Systems handle PSV by directly linking up with licensing bodies and certification boards. VerityStream gives you API connections in real time. Platforms like Credly and VerifyEd use blockchain technology for immediate, tamper-proof validation—handy for online learning and training setups. - Workflow automation and simplified onboarding
Drag-and-drop workflow builders, bulk credential issuing, built-in committee approval, and e-signature support make it easier to process high volumes quickly and accurately. Symplr Provider and MedTrainer offer customisable workflows suited to both hospitals and e-learning providers. - Integration and data compatibility
Plug-and-play integration with EHRs like Epic and Cerner, HRIS systems such as Workday or ADP, plus support for LMS, CAQH ProView, SSO (OAuth/SAML), cloud document storage, audit trails, and role-based access. Symplr Provider and MedTrainer cover these integration bases well to ensure secure, compliant operations. - User experience
Look for intuitive dashboards, self-service provider portals, mobile app access (iOS/Android), and region-specific permissions. Modio Health and MedTrainer deliver great mobile functionality, making compliance tracking simple whether you’re on-site or remote. - Scalability
Batch-friendly options like VerifyEd’s pay-per-credential approach, starting at £0.75 per credential for volume usage, are critical. Credly offers a similar batch system for digital badges, making scalability non-negotiable for organisations issuing thousands of credentials. - Advanced features
Secure digital wallets and instant verifications keep users motivated and streamline employer checks. VerifyEd stands out for enabling portable credential storage—a feature not yet common among rivals.
Whenever you’re weighing up systems, visuals like comparison tables really clarify which tools ace renewal alerts, speed, integration range, and mobile support. Zeroing in on these criteria means both healthcare employers and training providers can choose solutions with real confidence.
And on that note, let’s dive next into the practical benefits these platforms bring—beyond ticking boxes.
VerityStream: Automating Credentialing & Compliance for Large Healthcare Organizations
How VerityStream Accelerates Provider Onboarding and Reduces Compliance Risk
Let’s take a closer look at VerityStream—known to many as CredentialStream by HealthStream—which is built from the ground up for large-scale healthcare organisations juggling high volumes of providers.
Picture its Provider Lifecycle dashboard as the nerve centre. Here, every step—right from initial data entry to confirming privileges—is orchestrated with a keen eye on saving time.
This isn’t just theory; real enterprise deployments have seen onboarding times shrink to 7–14 days, making it possible for providers to start practising and billing with impressive speed.
Case studies demonstrate that strategic technology implementations can successfully reduce both the time and cost associated with provider onboarding.
Automated, configurable workflows are a huge part of that. They trigger renewal alerts for licences or certificates—typically 90, 60, or 30 days out.
The system sends reminders if any important document is missing or at risk of expiring. With bulk import tools onboard, you can migrate or add 500+ providers at a time.
Every change is logged with detailed audit trails and version control to keep compliance watertight.

Real-Time Credential Verification & Compliance Automation
Keeping everything air-tight and compliant is key. Primary source verification (PSV) links up with OIG, SAM, and medical boards via automated nightly API sweeps.
The results pop up instantly in the Credential Status dashboard, quickly flagging any sanctions or exclusions so nothing gets missed.
VerityStream’s patented automation checks provider data against compliance lists from TJC, NCQA, CMS, and URAC. This delivers out-of-the-box support for NCQA standards.
Need to show your audit trail? You can export compliance packages (PDF/CSV) for inspection and always know where you stand.
If you’d rather not handle verification in-house, HealthStream’s NCQA-certified CVO partners right in for a hands-off solution.
Integration, Security, and Scalability
VerityStream is designed to fit in with your existing systems. Expect native integration with Epic, Cerner, and HRIS giants like Workday and Oracle.
Real-time provider data sync works across multiple sites, powered by RESTful API and HL7 connections.
In 2025, enterprise users are seeing a 95% integration rate.
Unified login with SSO (OAuth and SAML) is standard, while bulk migration and export options support organisations scaling up or shifting regulations.
Security’s front and centre, too—HITRUST r2 and SOC 2 compliance ensure data stands up to even the toughest regulatory tests.
Pricing and Modularity
Pricing with VerityStream won’t look the same for every client—it’s quote-based.
Most large organisations spend between $25,000 and $150,000 annually, depending on provider numbers and which modules are active.
With its modular design, you can start small—just credentialing or analytics, for example—and grow as your needs get more complex.
Enterprise Results and Key Differentiators
What does all this translate to in the real world? Enterprises report 30% faster onboarding and 50% fewer compliance errors.
Audits are less stressful thanks to instant reporting. It’s the automation and unified data that drive day-to-day efficiency.
Automated credential monitoring streamlines the entire process by consolidating data from various sources into a single, unified platform. This provides a real-time, comprehensive view of a provider’s credentials, ensuring that your organization is always audit-ready.
Deep EHR and HRIS integration, robust bulk onboarding capabilities, and industry-standard security set VerityStream apart.
Looking for even more flexibility—say, for highly customised payer processes or gigantic renewal batches? That’s where symplr Provider shines.
We’ll get into those details next, so you can see how different platforms stack up for specialised needs.
symplr Provider: Enterprise-Scale Credentialing and Compliance
Key Workflow and Operational Impact
Let’s talk about symplr Provider—a cloud-based platform built for healthcare systems and payer organisations managing anywhere from 1,000 to over 25,000 providers.
You’ll usually find credentialing teams using it to handle multi-site onboarding, privilege assignments, and automating compliance across broad networks.
It’s well established in major health systems across the US and UK, bringing everything together for up to 250 facilities. That’s a big deal when it comes to streamlining what often becomes a maze of paperwork and email chains.
But how does the workflow really play out?
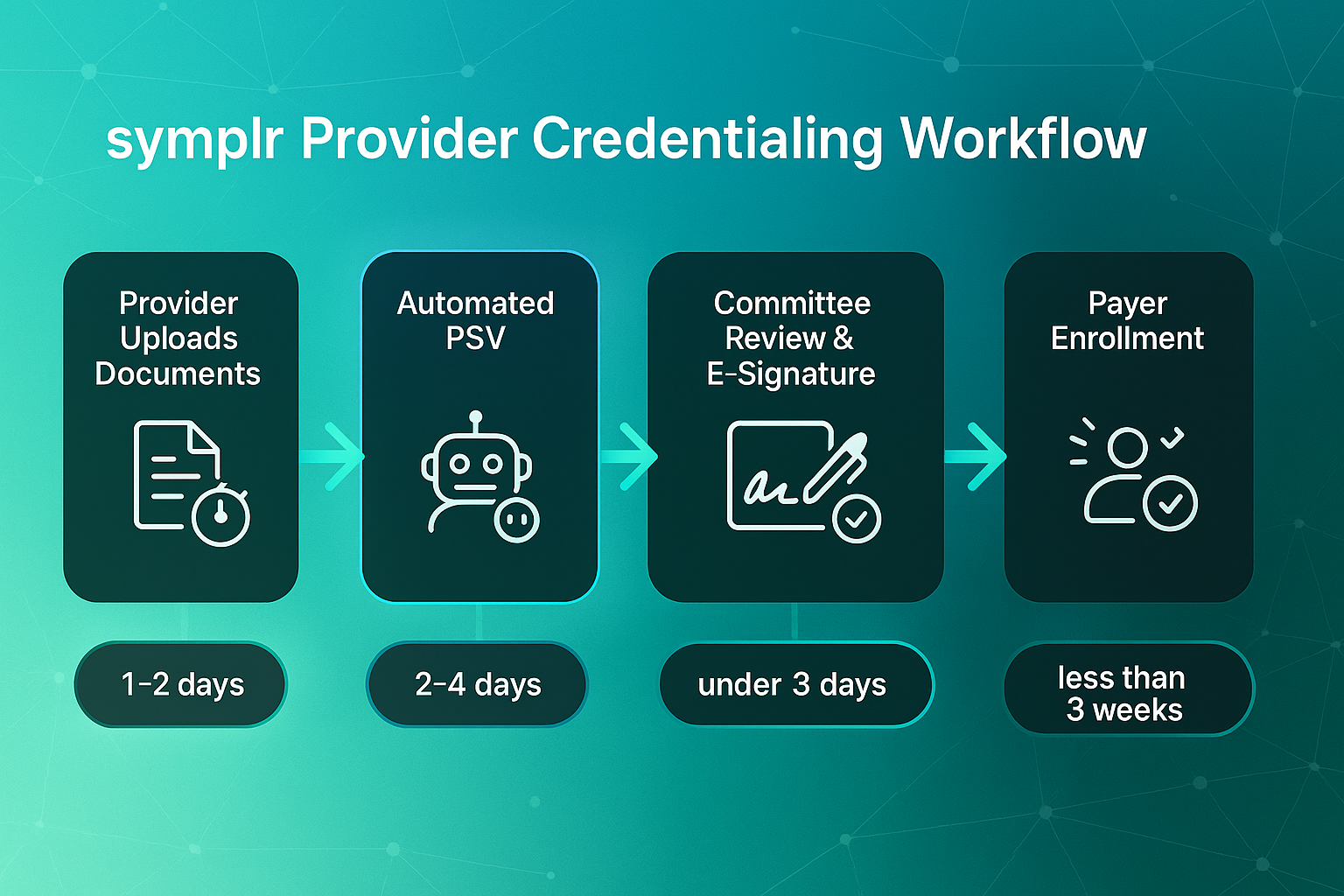
symplr Provider starts you off with a self-service portal. Providers upload their documents and fill in forms online—and here’s the best part, most are done in just one or two days.
Next, the platform’s automated primary source verification (PSV) checks credentials directly with databases like DEA, NPDB, and SAM.
This slashes those old manual turnaround times of about ten days down to 2–4 days.
After PSV, profiles go straight through automated review and committee sign-off with electronic signatures through DocuSign.
It’s efficient: the average profile goes from upload to sign-off in under three days.
Credentialed profiles then trigger payer enrolment alongside real-time status updates into EHRs (Epic, Cerner, Meditech) and HRIS systems (Workday, Oracle). The result is onboarding-to-billing happening in less than three weeks—not the six-week slog most teams know all too well.
Everything gets monitored on an ongoing basis, with automated reminders (at 90/60/30 days) and full audit logging for robust regulatory reporting.
Features, Integration, and Compliance
The platform offers a secure document repository, drag-and-drop workflow builder, automated exclusion checks, and real-time compliance dashboards.
Bulk onboarding? No problem—symplr Provider can process up to 10,000 providers in one go.
It communicates directly with key databases: EHR, HRIS, CAQH, and payers, so administrative overhead shrinks noticeably.
And with mobile portals, providers get easier, on-the-go access. Benchmarks show a 40% drop in onboarding inquiries once mobile is in play.
Users report some dramatic results, with credentialing process times cut by 60–75% and audit pass rates rising from 87% to over 98%.
A case study on a Southern U.S. healthcare organization found that implementing a cloud-based credentialing platform boosted the timeliness, accuracy, and efficiency of their provider management processes.
For extra peace of mind, there’s the Credentials Verification Organization (CVO), letting organisations outsource NCQA-certified PSV, alongside role-based access for privacy and compliance alignment.
Pricing and Best-Fit Scenarios
symplr Provider operates on a subscription model, typically costing $3 to $9 per user monthly—think bulk discounts for larger teams or annual contracts.
It’s a strong match for health systems needing rapid, compliant onboarding at scale.
Especially if you’re consolidating several sites or pushing to speed up reimbursement cycles, this platform brings genuine value.
Nevertheless, there are areas where other credentialing platforms may offer features that symplr Provider does not.
You won’t get blockchain-based credential verification, digital wallets, or portable badge issuance here. That’s the territory of platforms like VerifyEd and Credly, which are better suited to organisations focused on digital portable credentials or education-first strategies.
Of course, if your interests skew toward distributed clinics, telehealth, and mobile-enabled credential management, keep an eye out—Modio Health OneView will be our next stop, and it promises some clever solutions for modern healthcare staffing.
Modio Health OneView: Credentialing Automation for Distributed Healthcare Teams
Essential Features and Compliance Integrations
If you’re working with a healthcare organisation that’s spread across multiple sites or deals with frequent staff turnover, Modio Health OneView is designed with you in mind. Its cloud-based system puts everything in one place—automated alerts for expiring credentials, centralised digital profiles for licences, CME (Continuing Medical Education) records, and compliance documents all within easy reach.
Building on this centralised convenience, a real standout is the way OneView taps directly into over 100 credentialing sources, such as the DEA (Drug Enforcement Administration), OIG (Office of Inspector General), and state medical boards.
What does that mean for you? Real-time, automated primary source verification (PSV) across the board.
This level of automated compliance monitoring goes a long way towards cutting out manual tracking and making sure you’re covered for every regulatory requirement, regardless of how many providers you manage.
Automation, Reporting, and Workflow
The heart of OneView really beats for administrative automation. You get expiry alerts tailored to each credential type and can set up forms that populate themselves—saving time and avoiding repetitive data entry.
Electronic signatures simplify onboarding and renewals, especially when you’re onboarding large batches of staff.
Providers can log in securely via their browser and update their own data. This means less admin back-and-forth and fewer mistakes.
This is especially handy if you’re managing agencies or telehealth teams with significant numbers.
Custom dashboards and exportable reports—whether in Excel, CSV, or PDF—let administrators monitor compliance status, CME attestations, and licence renewals at a glance.
Everything’s tracked through detailed audit logs, giving you transparency for audits and ensuring full NCQA (National Committee for Quality Assurance) compliance.
Integrations, Security, and Support
OneView isn’t just about credentialing—it’s about fitting in seamlessly with the systems you already rely on. Expect integration with HR, EHR, and practice management platforms, which keeps information flowing smoothly throughout your operations.
Single sign-on SAML 2.0 and SOC 2 Type II certification put data protection front and centre, a must if you’re handling sensitive health information.
For those inevitable busy waves—think onboarding spikes or contract staff—Modio also offers Extended Credentialing Services teams who step in and handle the extra load.
That can be a real lifesaver for flexible staffing agencies ramping up quickly.
Pricing, Ideal Use Cases, and Decision Points
Modio Health OneView’s pricing flexes with organisational size and needs, so you won’t be forced into a one-size-fits-all package.
Even entry-level tiers have no setup fee, helping practices get started with minimal fuss.
Distributed networks, fast-growing clinics, and telehealth or staffing agencies often find this platform particularly effective.
Key strengths include robust primary source verification automation, strong security, intuitive self-serve provider tools, and responsive support.
While it doesn’t offer highly customisable ad hoc reporting or direct online application processing, its commitment to compliance reliability and regular, partner-driven feature improvements really sets it apart.
For healthcare groups needing real-time compliance, streamlined automation, and solid oversight across many sites or providers, Modio Health OneView stacks up as a strong option in 2025’s credentialing software landscape.
Now, if your requirements lean toward highly specialised credentialing workflows, keep reading—the next section explores how IntelliCred might offer what you’re after.
IntelliCred (IntelliSoftGroup): Customisable Credentialing for Complex Healthcare Needs
Let’s take a closer look at IntelliCred from IntelliSoftGroup—a platform built for healthcare organisations that operate in especially demanding or ever-changing credentialing environments. If you’re juggling sites in different regions, managing credentialing for multiple clients as a CVO (Credentialing Verification Organisation), or overseeing a sprawling workforce for a health plan or staffing agency, spot solutions just don’t cut it. You need flexibility. That’s exactly what IntelliCred delivers through its dynamic credential library and real-time “Credentialing Status Tracker”.
Unlike older systems tied to static templates, IntelliCred enables you to adapt credential types and requirements as new regulations emerge or policies update. The dashboard puts organisation-wide compliance at your fingertips, which is a huge relief when each department, site, or client operates under different rules.
Who Benefits and When to Choose IntelliCred
There’s no denying that IntelliCred is engineered for complexity. It’s not meant for single-site clinics with fixed checklists. It comes into its own when organisations face shifting standards, massive onboarding initiatives, or real-time demands on compliance visibility.
For example, one large multi-speciality hospital processed more than 150 provider applications at once using IntelliCred’s bulk onboarding and analytics tools, which led to a 40% decrease in onboarding time and faster claims processing. That’s a real operational win.
So, in which scenarios does IntelliCred deliver the most impact? Whenever you’re dealing with a fast-changing regulatory climate or frequent structural changes, this system gives you control and agility. Before listing the main signals that it could be your best fit, let’s get clear about what makes these triggers so crucial: they’re reflective of environments where inefficiency or compliance risk can cause real pain—operationally and financially.
Organisations typically consider IntelliCred when the following needs arise:
- Unlimited, custom credentialing workflows
are required for new sites or frequently updated specialty rules. - Different regulatory standards
There is constant management of different regulatory standards across regions, departments, or facility types. - Decision-makers must have real-time analytics
on credential status, compliance backlogs, or upcoming bottlenecks to guide priorities.
When your world demands adaptable oversight and swift response, that’s where IntelliCred really shines.
Core Features, Workflow Automation, and Analytics
The true power of IntelliCred sits within its Workflow Configurator and the depth of its analytics.
When administrators can launch, edit, and redeploy credentialing processes instantly, the risk of lagging behind new requirements is dramatically reduced.
Rapid workflow changes, compliance alignment, and responsive reporting become everyday advantages.
To appreciate why this matters, consider how the following features work in practice. These are tuned for operational scale and regulatory variation:
- Dynamic Credential Library
Admins can create, change, or retire credential types on the fly, ensuring every workflow stays compliant. - Bulk Onboarding
Process up to 200 provider applications at a time, efficiently delegated by site, department, or committee. - Automated Primary Source Verification (PSV)
Automated overnight checks with OIG, SAM, NPDB give peace of mind, with instant “Sanction Alert Reports” if issues pop up. - Credential Expiry Calendar
The colour-coded dashboard helps avoid missed renewals, which one case study showed dropped by 90% post-adoption. - Advanced Analytics
Monitor turnaround times, renewal backlogs, and risk. Export full audit trails (PDF/CSV) for regulatory reviews and continuous improvement.
Integration, Mobile Support, and Data Management
For modern healthcare networks, integrated data flows and mobile access are more than “nice-to-haves”—they’re essential for keeping everyone on the same page.
IntelliCred plugs straight into Epic, Cerner, Workday, and Oracle, using HL7 and FHIR to keep EHR and HR data in sync.
Admins and providers get secure mobile access via native iOS and Android apps. Authentication is handled through SAML 2.0 and OAuth2 single sign-on, and permissions can be as granular as you need, right down to specific departments or committees. Batch importing and exporting by Excel, XML, or JSON adds another layer of operational convenience.
Implementation, Pricing, and Differentiators
Launching IntelliCred is straightforward: most organisations are live in 60–90 days, with onboarding support throughout.
Pricing starts at $29/month (Standard), $199/month (Premium), and $0/month (Individual, 2024), with custom options available for large-scale needs.
The system upholds NCQA alignment and produces export-ready audit trails that simplify regulatory reporting.
But IntelliCred’s real edge? It combines workflow agility, real-time analytics, and robust integrations, making it possible to manage up to 200 provider onboardings each cycle.
If navigating complexity, fast change, or compliance risk is your everyday, this is a solution built for you. And as we switch gears, the next section explores how digital credential portability is changing the landscape for both healthcare employers and staff.
CredentialStream by HealthStream: Best-Fit Scenarios, Core Benefits, and Where It Shines—Or Doesn’t
CredentialStream by HealthStream is more than just a credentialing system. It is a solution shaped for healthcare staffing and compliance at scale.
For growing clinical groups and large multi-site health systems, CredentialStream simplifies administration, tightens compliance, and speeds up provider onboarding.
Its powerful fit, however, isn’t ideal for every organisation.
Where CredentialStream Excels
There are clear situations where CredentialStream stands out, especially for operationally complex organisations.
- Multi-site health systems
Centralises credentialing for 3 to 250+ facilities in multiple states, streamlining oversight throughout the year. - Fast-growing clinics and hospital networks
Handles onboarding of dozens or hundreds of providers each month, ensuring compliance across states and payers. - Regulatory-heavy onboarding teams
Monthly software and workflow updates align with changing requirements of NCQA, TJC, CMS, and URAC. - Mixed provider rosters
Adapts credential requirements for physicians, locums, nurses, and allied health professionals, no matter how often regulations change.
If your organisation rarely hires new staff or focuses only on digital badges rather than live provider onboarding, these real-time tools may be harder to justify.
CredentialStream: Main Benefits
Healthcare teams report several measurable improvements using CredentialStream.
- Rapid onboarding
Credentialing times reduced by 25–50%. Staff often complete onboarding in 10–15 days instead of a month. - Audit-proof compliance tracking
Exportable audit trails and dynamic dashboards provide live compliance visibility for NCQA and URAC inspections. - Workflow automation
Pre-built templates keep credentialing processes aligned with changing regulations, avoiding tedious yearly manual overhauls. - Scalability
Suitable for organisations from a single site to large networks up to 250 sites. - Mobile and self-service portals
Providers can update their own credentials via web and app tools, reducing administrative back-and-forth by up to 40%.
In addition to these benefits, onboarding teams can typically go live in 30–90 days. The platform’s knowledge base supports both navigation and regulatory audit walkthroughs.
Deep Electronic Health Record (EHR) integrations may extend launch time, but most groups start fast.
Pricing, Modules, and Tangible Value
When evaluating pricing and overall value, it’s important to note that CredentialStream is quote-based. Annual costs generally range from $25,000 to $150,000, depending on staff numbers, facilities, and selected modules.
These modules add flexibility, with add-ons like privileging, analytics, e-signature support, and payer enrolment available.
High-volume teams can benefit from bulk pricing, which lowers per-provider costs.
Alongside this, mobile portal adoption slashes admin workloads. Hospitals report 10–20% reductions in indirect costs when providers self-update their information.
Who Shouldn’t Choose CredentialStream?
In some cases, CredentialStream may not be the right choice.
- Stable and rarely-changing staff rosters
Organisations with minimal staffing changes may be better served by leaner, lower-cost solutions with basic tracking. - Education-only or digital badge programmes
Lacks features for digital badge or education-focused credentialing offered by platforms like Credly or VerifyEd. - Basic standalone needs
If all you need is static tracking and don’t require deep integration, audit tools, or monthly regulatory updates, simpler software may suffice.
At-a-Glance Key Takeaways
Here’s a summary of who gets the most value from CredentialStream:
- Multi-site and multi-specialty teams
Benefit from centralised oversight and rapid, compliant onboarding. - High-churn clinical networks
Monthly regulatory updates help reduce compliance risk. - Hospitals needing instant audit readiness
Generates on-demand reports for NCQA, TJC, and CMS audits.
For single-site groups with static rosters, a simpler, basic solution may be sufficient.
Healthcare staffing and compliance expectations are constantly changing. Matching your software’s capabilities to your organisation’s needs is vital.
The next section will explore digital badge and portable credentialing solutions designed for a modern, mobile workforce.
Silversheet: Streamlined Credentialing for Small and Mid-Sized Clinics
There’s no sugar-coating it: countless outpatient clinics and ambulatory centres still cling to spreadsheets for tracking credentials—a risky move that often leads to missed renewals and surprise penalties.
Fast forward to 2025, and these small clinics face a parade of NCQA, CMS, and Joint Commission audits every year.
That’s where Silversheet steps in: a browser-based platform built for clinics with fewer than 500 staff, promising quick setup and instant compliance dashboards to take the pain out of credentialing.
Credential Management Automation and Compliance Outcomes
With Silversheet, you’re no longer chasing paper trails or juggling sticky notes. Expiring licences, DEA registrations, board certifications, CAQH records, and malpractice insurance are all tracked automatically.
Admins can set up renewal reminders—90, 60, 30, or 15 days out—that show up both in email and on the dashboard.
This automated system leads to real results. Clinics running Silversheet saw missed renewals drop by 80 percent compared to old manual methods.

Every document upload is HIPAA-compliant, and there’s enough secure storage for all your providers, up to 500, without extra charge.
Even better, every change is audit-tracked to keep NCQA, URAC, and Joint Commission requirements at the forefront.
Most clinics hit green dashboard status—meaning all credentials are current—within two to seven days of moving their data over.
Usability, Deployment, and Core Technical Specifications
Silversheet’s browser experience is designed for clarity and speed. The dashboard uses colour-coded fields for each provider, including name, licence type, last verified date, upcoming expiry, and overall compliance as green, yellow, or red.
Approvals only take two or three clicks, so you’re not bogged down in forms. Full system rollout happens fast—usually within twenty-four to seventy-two hours.
Admins get up to speed with just ninety minutes of training. Providers can self-onboard securely with step-by-step prompts.
All major functions work via any browser, including iOS and Android. There’s no dedicated mobile app, but real-time credential status and flexible reminder settings help keep no one in the dark.
For teams looking for seamless usability, these features offer instant visibility to credential status and a hassle-free onboarding process.
Integration Details
When it comes to connecting with your other systems, Silversheet plays well with the big EHR players: Epic, Cerner, AthenaHealth, and Merge.
This is made possible thanks to RESTful API and FHIR v4.0.1 support.
HRIS systems like BambooHR, ADP, and Workday link in through middleware. These integration capabilities make it easier to connect credentialing with your HR operations.
However, working with older or partial EHRs can mean extra hassle. If your team lacks capacity for SOAP protocol or custom API tweaks, you may find some integration limitations.
In those cases, considering support or alternative solutions is worthwhile to ensure smooth deployment.
Pricing, ROI, and Fit
Let’s talk money and results. Silversheet keeps it simple with pricing at thirty-five to sixty dollars per user per month, tier-based.
For a typical clinic with two to four admins and twenty to forty providers, the bill usually lands between one hundred twenty and one hundred eighty dollars per month.
Large teams on the unlimited provider tier pay forty-nine dollars per user per month. There are no installation fees, saving up-front costs.
Building on this, the platform starts to show a return for smaller clinics with less than one hundred fifty staff within six to twelve months.
Audit pass rates often climb from sixty-eight percent to ninety-three percent in the first year post-adoption.
Instant audit readiness is a win, but you won’t find advanced mobile workflows or custom analytics here.
Other platforms such as Modio, symplr, and IntelliCred cover those bases for clinics with more complex requirements.
Best Use Cases and Limitations
Silversheet shines for outpatient clinics, surgery centres, and physician groups needing quick deployment, solid compliance, and minimal IT fuss.
But if your clinic needs deep custom analytics, robust mobile apps, or hardcore integration with legacy systems, you may want to scope out Modio Health OneView, IntelliCred, or symplr Provider for more specialised features.
Looking forward, the next section will break down portable credentialing and instant badge verification—two essentials for healthcare education providers and MOOCs in today’s credentialing landscape.
VerifyEd: Digital Credentialing for Healthcare Education & MOOCs
Platform Overview, Best-Fit Scenarios, and Boundaries
Let’s get into how VerifyEd fits into the digital credentialing space, especially for healthcare education and MOOC (Massive Online Open Course) providers.
This solution is purpose-built for organisations that need to send out digital certificates, badges for CPD (Continuing Professional Development), specialist skills, or course completions at scale—think regulatory refreshers like CPR or ACLS.

That means if your primary need is quick, secure recognition of learning achievements or regulatory updates, this is precisely its territory.
But it’s not a tool for full hospital HR management or ongoing provider onboarding—those are best left to platforms focused on licensure tracking and employment compliance.
The real sweet spot? Healthcare training providers, universities, and those digital platforms delivering high-volume qualifications.
If you’re looking to motivate learners or show their value to healthcare employers, VerifyEd delivers a concrete solution.
Standards, Technical Specifications, and Integration
On the technical front, VerifyEd credentials are built on the Open Badges 2.0 standard (essential for digital certificates), and reinforced with blockchain for tamper-evidence.
Credentials export in CSV, PDF, and JSON-LD formats, so data moves smoothly anywhere it’s needed.
Recipients aren’t left juggling files—they can drop proof straight into digital wallets, LinkedIn profiles, or attach it to job applications.
Integration isn’t a headache, either: platforms like Workday, BambooHR, and SAP SuccessFactors are all supported.
The authentication process is simple and secure, using unique verification links or QR codes embedded on digital awards.
Blockchain Verification and Outcome Specifics
Here’s where VerifyEd changes the game.
Each credential is validated in real-time on the blockchain.

When an employer or certifying body clicks through the verification link or scans a QR code, it’s instant: they’re met with a page showing all credential details, a blockchain authenticity stamp, and the unique transaction ID.
Employers love the “Verified on Blockchain” badge, plus all the export options—everything’s downloadable as PDF or JSON-LD.
That green checkmark tells them the credential is valid and active.
And—perhaps best of all—the entire process takes just five seconds, no more waiting days for results or chasing paperwork.
Pricing, Scalability, and Credential Portability
VerifyEd charges per credential. For organisations with big batch volumes, costs drop as low as £0.75 each, with no long-term contracts required—a clever option for pilot projects or major annual programmes.
Credential holders, meanwhile, get true portability: they can share digital awards with wallet apps, LinkedIn, or by simple downloads.
Every major format is supported, so employers and platforms have zero compatibility worries.
Analytics and Platform Limitations
Admin dashboards reveal issuance volume, basic learner activity, and how often credentials are verified by third parties or employers.

But let’s keep it practical: advanced analytics—like predictive dropout risk—or regulatory reporting for HR are not standard.
If compliance submission or renewal tracking is on your radar, it’s best to pair VerifyEd with a classic provider credentialing system.
In short, VerifyEd helps healthcare course providers and educators issue verifiable, portable, blockchain-secured digital credentials—fully aligned to global standards.
Employers and auditors get instant, reliable proof—usually a green tick and all supporting data—streamlining what used to take days into mere seconds.
Looking to improve your course sales, marketing & experience?
Book a free course optimisation strategy call with one of our specialists.
Book a call
Why the Best Credentialing Software Matters
Credentialing isn’t just a compliance checkbox—it’s the foundation of trust, safety, and operational efficiency in healthcare. The right software doesn’t just automate paperwork; it actively reduces risk, accelerates onboarding, and gives your team the confidence to face audits and regulatory changes head-on.
If you’re weighing options, I recommend mapping your biggest pain points—whether it’s multi-site complexity, high-volume onboarding, or digital badge issuance—against the strengths of each platform. Consider these next steps:
- List your must-have features: automation, integration, mobile access, or real-time analytics - Assess your scale: small clinic, distributed network, or education provider - Request demos and trial periods to see real workflows in action
No single solution fits every scenario, but choosing credentialing software that adapts as your needs evolve is the smartest investment you can make. In healthcare, reliable credentialing isn’t just about passing audits—it’s about protecting your people, your reputation, and your future.
.svg)




.png)

